Entire chronic pain research division eliminated in NIH layoffs
Last week, the Department of Health and Human Services experienced a significant blow with a series of layoffs that resulted in the elimination of an entire division dedicated to researching pain. The National Institutes of Health Office of Pain Policy and Planning, which was responsible for coordinating pain-related research across the federal government, saw all but one full-time position cut as part of the reduction in force implemented by Health Secretary Robert F. Kennedy Jr.
This move leaves a gaping hole in the government-backed scientific community, as none of the NIH’s 27 institutes are solely focused on pain research. This fragmentation in research efforts surrounding both acute and chronic pain, as well as the physiological causes and health outcomes associated with pain, is concerning given that pain is considered the country’s most common disabling condition. According to the Centers for Disease Control and Prevention, 17 million people in the United States experience “high-impact” chronic pain.
Advocates and experts in the field, such as Kate Nicholson, founder of the nonprofit National Pain Advocacy Center, emphasize the importance of understanding and addressing chronic pain, which is a widespread health problem and a leading cause of long-term disability globally. Despite its prevalence and impact on individuals and society, chronic pain has historically been misunderstood and under-treated.
The dismantling of the NIH’s pain office raises concerns about the future of crucial research projects and the coordination of efforts between different NIH institutes and government agencies. The office, located within the National Institute of Neurological Disorders and Stroke, collaborated with various entities such as the National Institute on Drug Abuse, National Cancer Institute, and the Substance Abuse and Mental Health Services Administration to advance pain research and clinical care.
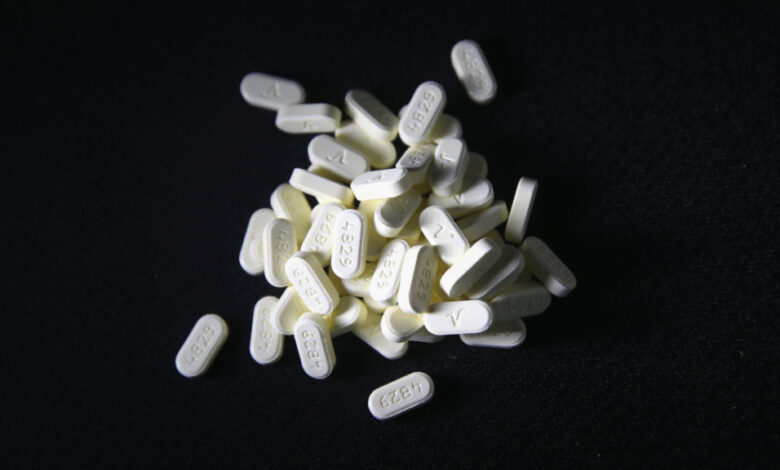
In the midst of the opioid crisis and heightened awareness of chronic pain, the NIH has been focusing on developing non-opioid painkillers to address addiction concerns. However, advocacy groups representing chronic pain patients have expressed worries about the potential negative consequences of restricting opioids too severely, such as reduced quality of life, increased reliance on illicit opioids, and even suicide.
The NIH’s pain office played a crucial role in coordinating initiatives like the HEAL Initiative, which aims to combat the opioid crisis by developing new addiction treatments and pain medications. Additionally, the office managed the Interagency Pain Research Coordinating Committee, a federal advisory group responsible for aligning pain-related scientific efforts across government agencies. The future of this committee is now uncertain following the closure of the pain office.
Experts like Robert Kerns, a Yale professor emeritus and long-time pain researcher, highlight the importance of retaining or replacing the functions of the pain agency to ensure the continuation of vital pain research and comprehensive efforts to address gaps in scientific knowledge. The loss of the NIH’s pain office poses a serious threat not only to pain science but also to the broader mission of addressing pain-related issues outlined in national strategies and reports.
As questions linger about the fate of the pain agency’s functions within the NIH or elsewhere in the federal government, advocates and researchers are left to wonder about the future of pain research and treatment in the United States. The closure of the NIH’s pain office underscores the challenges faced by those dealing with chronic pain and the urgent need for continued support and investment in pain research and care. The world of technology is constantly evolving, with new innovations and advancements being made every day. One such innovation is the development of artificial intelligence (AI) systems, which are designed to mimic human intelligence and perform tasks that would normally require human intervention. These AI systems have the potential to revolutionize industries and improve efficiency in a wide range of applications.
One area where AI technology is already making a significant impact is in the healthcare industry. AI systems are being used to analyze medical images, such as X-rays and MRIs, to help doctors diagnose diseases more accurately and quickly. These systems can detect patterns and abnormalities that may not be immediately apparent to the human eye, leading to earlier detection of diseases and better treatment outcomes for patients.
In addition to medical imaging, AI technology is also being used in drug discovery and development. AI systems can analyze large amounts of data to identify potential drug candidates and predict their effectiveness, reducing the time and cost of bringing new drugs to market. This has the potential to revolutionize the pharmaceutical industry and accelerate the development of new treatments for a wide range of diseases.
AI technology is also being used to improve patient care and outcomes. AI-powered chatbots and virtual assistants can provide patients with information and support, helping them manage their health and navigate the complex healthcare system. These systems can also analyze patient data to identify trends and patterns that may indicate potential health issues, allowing for earlier intervention and better outcomes.
However, the use of AI technology in healthcare is not without its challenges. Privacy and security concerns are paramount, as AI systems must be able to protect patient data and comply with strict regulations. Additionally, there is a need for greater transparency and accountability in the development and deployment of AI systems, to ensure that they are safe, effective, and ethically sound.
Despite these challenges, the potential benefits of AI technology in healthcare are vast. By harnessing the power of artificial intelligence, we can improve diagnosis and treatment, accelerate drug discovery, and enhance patient care. As the technology continues to advance, the future of healthcare looks brighter than ever before.




