In a broken mental health system, a tiny jail cell becomes an institution of last resort
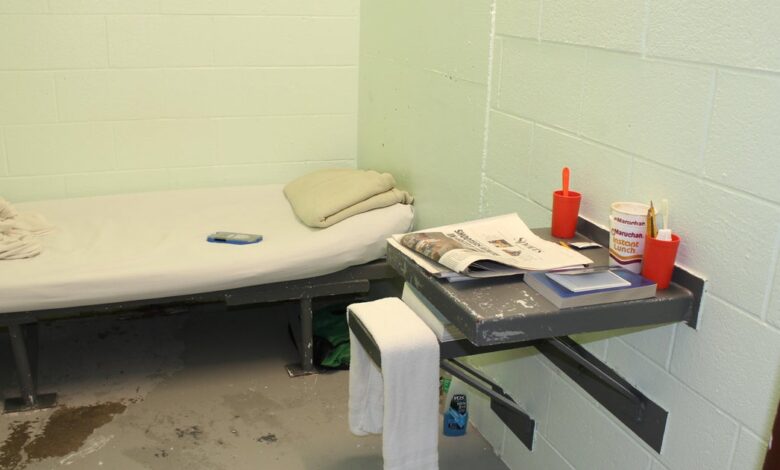
Polson, Montana — In the small northwestern Montana town of Polson, individuals accused of crimes and in need of mental health care often find themselves confined in a basement jail cell the size of a walk-in closet. These prisoners, some held in isolation for months, have left their mark on the metal door’s brown paint, with scratched initials and the haunting phrase “love hurts.” Pacing back and forth in the cramped space, they await their fate in a state of limbo, not convicted of a crime but deemed unstable for release. Sleeping on a narrow cot beside a toilet, their only view is a dimly lit hallway visible through a small window in the door.
Last year, a man sentenced for stealing a rifle spent 129 days in one of these cells, waiting for a spot to open at Montana’s only state-run psychiatric hospital. Another man in a neighboring cell faced a similar waitlist lasting roughly five months, enduring frequent restraints in an emergency chair designed to subdue him during psychotic episodes. Despite regular visits from the jail’s mental health doctor, his condition continued to deteriorate, leading to distressing episodes that prompted him to seek confinement in the restraint chair until he calmed down.
County Attorney James Lapotka expressed his concerns about the inhumane conditions, stating, “Somebody who’s having a mental health crisis — they don’t belong here. We don’t have anywhere else.” Unfortunately, this situation is not unique to Polson, as communities across the country struggle to provide adequate mental health services, especially in times of crisis. Nearly half of the individuals incarcerated in local jails in the U.S. have a mental illness, highlighting the urgent need for reform.
Montana’s challenges in addressing mental health crises are exacerbated by the lack of resources and facilities to accommodate those in need. With the Montana State Hospital often at full capacity and few local hospitals equipped with inpatient psychiatric beds, individuals arrested for various offenses can languish in jail for extended periods, exacerbating their mental health issues. Despite years of awareness about this issue, state officials have struggled to find viable solutions, citing staffing shortages and funding constraints as significant barriers.
In an effort to address the crisis, the Montana Department of Public Health and Human Services has proposed legislation to shield the state from liability for delays in mental health care when the state hospital reaches full capacity. Additionally, $6.5 million in grants have been made available to establish jail-based mental health stabilization services, aiming to provide more immediate care to those in need.
While state officials and advocates work towards long-term solutions, the immediate reality for individuals in crisis remains bleak. Vincent River, the jail’s sole mental health clinician, struggles to secure psychiatric care for inmates due to the limited availability of psychiatric beds in Montana. As a result, many individuals are left to deteriorate in isolation, without access to proper treatment or medication.
Efforts to fill these gaps, such as the launch of a mobile team staffed by individuals with lived experience of mental health challenges, offer some hope for improved care. However, the stark choice between confinement in a jail cell or an overcrowded emergency room underscores the urgent need for comprehensive reform in Montana’s mental health system.
As the state grapples with these complex challenges, the promise of increased funding and support from Governor Greg Gianforte offers a glimmer of hope for a brighter future. However, the road to rebuilding Montana’s behavioral health system and providing quality care for those in crisis is fraught with obstacles that will require sustained effort and collaboration from all stakeholders involved.
Despite the picturesque surroundings of Polson and its proximity to natural wonders like Glacier National Park, the stark reality of inadequate mental health care looms large in the community. As local officials and advocates continue to push for meaningful change, the urgent need for accessible, compassionate mental health services remains a pressing concern in Montana and beyond.
KFF Health News is a national newsroom dedicated to producing in-depth journalism on health issues and is a core program at KFF — the leading source for health policy research, polling, and journalism.





